Osteoarthritis is the most common joint disorder in the United States and may cause pain, stiffness, and limitations with day to day activities. Unfortunately, many people feel forced to give up their favorite sports or lifestyle as a result of being labeled with “osteoarthritis”.
A diagnosis of “osteoarthritis” can be confusing.
What does it mean? Does it mean you can’t bike, hike, walk, or exercise without pain? How should you treat it and what can you do to prevent it from getting worse?
What is Osteoarthritis?
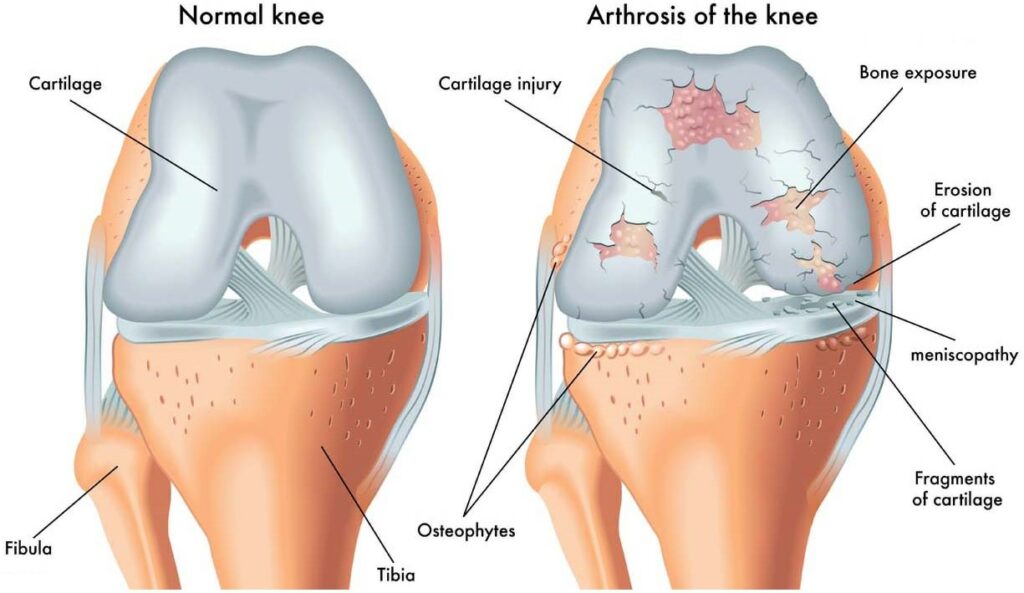
Osteoarthritis, also known as degenerative joint disease, occurs when the cartilage that covers the ends of the bones in your joints gradually deteriorates. Typically affecting weight bearing joints, such as the knees, hips, and hands, the degenerative process causes thinning of the cartilage, narrowing of joint spaces, and decreased cushion between bones. This breakdown process puts more pressure on the sensitive surface of the bones within the joint, causing inflammation, pain, bone spurs, and further wear-and-tear of the joint.
Being diagnosed with osteoarthritis does NOT mean that you cannot or should not live or enjoy an active lifestyle. On the contrary, activity can actually improve symptoms of osteoarthritis and slow down or stop the progression of it. Many people with osteoarthritis live an active, healthy lifestyle, without limitations.
How is Osteoarthritis diagnosed?
Osteoarthritis affects over 32.5 million Americans and is usually diagnosed by physical examination and an x-ray. From the x-ray imaging, physicians will look for reduced spacing between bones within the joint and signs of inflammation. They will look at how much cartilage is in the joint to protect the underlying bone from further wear and tear. They will also look for any bone fragments or “spurs” poking up into the joint that can cause more pain.
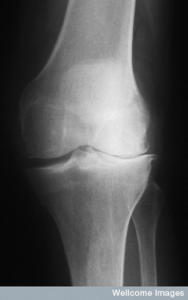
X-ray findings should be compared with a physical exam to assess for actual loss of joint range of motion, stiffness, weakness, and activity limitations before a treatment plan is determined.
Did you know that there are people with osteoarthritis who are NOT symptomatic? They have no pain, stiffness, swelling, or limitations associated with the condition. In fact, they might not even know that they have it!
Evidence of degenerative joint changes can be seen in young adults to older adults, but the risk of developing osteoarthritis increases with age.
Some of the risk factors contributing to development of OA include:
- Age (over 60 years old)
- Genetics
- Being a female
- Being overweight
- Having a pre-existing knee injury
- Overuse of the knee or hip joint
- Muscle weakness surrounding the joint
Does Osteoarthritis always get worse?
Osteoarthritis is a progressive condition that continues to worsen if nothing is done to reduce pressure and wear-and-tear on the joint.
Joint wear-and-tear that causes inflammation, swelling, and stiffness leads to more weakness, further breakdown, more stiffness, and more limitations. The cycle continues if no change is made to break the cycle.
While there is no cure for OA, it is possible to slow or stop the progression of osteoarthritis through appropriate intervention…and most people don’t realize this!
Someone with OA may experience periods of “flare-ups,” where the joint suddenly becomes swollen, stiff, and/or painful. There may also be periods where symptoms resolve, range of motion is restored, and the joint feels relatively normal.
Controlling the “controllables” is an important tactic in managing osteoarthritis, so the periods of flare ups don’t get worse than they need to be. Knowing what to do to calm a flare-up is an important step in long-term management and will aid in continuing to do the activities and sports that you love.
Normal range of motion (ROM) helps to spread out the forces on the joint; Good STRENGTH helps to support the joint; and good MOVEMENT PATTERNS help to reduce abnormal forces on the joint. These concepts are the basis of what will SLOW or STOP the worsening of degenerative joint disease.
Losing weight if overweight, strengthening the musculature surrounding the hip and knee, maintaining mobility and flexibility, and controlling inflammation and pain are important strategies in preventing osteoarthritis from worsening.
Common Treatments for Osteoarthritis
Activity
While it might seem that activity can cause more pain and swelling at first, physical activity is actually proven to reduce symptoms and improve quality of life for people with degenerative joint disease. Movement promotes circulation and can lead to more pain-free days. Of course, you will need to make sure that you are choosing the right activity, progressing appropriately, and listening to your body.
A great place to start is by improving mobility and flexibility with simple stretches.
Physical Therapy
Physical Therapy is proven to alleviate symptoms, increase activity tolerance, and improve quality of life for people with osteoarthritis through a structured approach to restoring range of motion, functional strength, and balance.
If you want to live an active lifestyle, play sports, and enjoy the outdoors, ACL STRONG provides a skilled exercise progression to strengthen your legs and core, improve balance and body control, and learn how to protect your body and lifestyle long-term. This is an online program and an excellent option if you want the convenience and freedom to exercise on your own at home, while still having expert guidance and support.
Injectables
Your physician may be willing to try a hyaluronic acid injectable into the affected arthritic joint. This fluid is similar in makeup to your body’s own synovial fluid, which is like oil in your car. An injectable can lubricate affected bone and joint tissue to decrease symptoms of osteoarthritis, which can allow you to be more comfortable and delay the need for surgery.
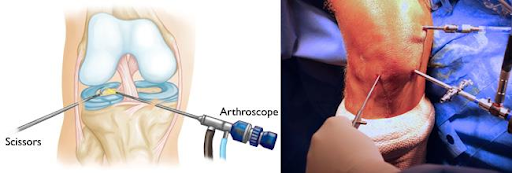
Arthroscopy
Arthroscopic surgery is an option when an orthopedic surgeon feels confident that symptoms can be decreased by cleaning up the surface tissue within the affected joint. An arthroscopic surgery is performed by placing small incisions into the joint to remove damaged tissue and create a smoother surface. The surgery will facilitate increased blood flow to the joint, which can help “restart” the healing process, reducing symptoms of osteoarthritis.
Joint Replacement Surgery
In cases where more conservative treatments have failed to alleviate symptoms and improve quality of life, joint replacement surgery may become the best option. Replacing the degenerated joint surface with mechanical parts can give you the restoration you need to be as active as you want.
Recovery from joint replacement surgery will involve several months of activity progression and physical therapy. While the timeline varies for everyone, most patients do return to normal activities and exercise, such as hiking, walking, biking, golfing, tennis, lifting weights, housework, and yardwork. With hard work, commitment, and consistency, many are able to return to their prior sports and higher level activities.
Osteoarthritis should NOT be daunting or intimidating. Receiving a diagnosis of osteoarthritis does not have to feel confusing.
👉 How you manage your condition is up to you. You CAN live an active, healthy, sporty lifestyle, with the presence of degenerative joint disease. Manage it with exercise, nutrition, making good choices, and expert support, and you can continue to live the lifestyle you choose. 💪